Clipboard, Search History, and several other advanced features are temporarily unavailable. Trigger point injections take about 30 minutes, and you can expect to go home on the same day. This site needs JavaScript to work properly. The rates 3 months after injection were 27 of 41 in the triamcinolone cohort and 22 of 31 in the dexamethasone cohort. A trigger point injection involves the injection of medication directly into the trigger point. Choice of Corticosteroid Solution and Outcome After Injection for Trigger Finger. On rare occasions, patients exhibit signs of anesthetic toxicity, including. Hand (N Y). Palpation of the trigger point will elicit pain directly over the affected area and/or cause radiation of pain toward a zone of reference and a local twitch response. Many drugs can affect dexamethasone. Decadron is also used to treat certain types of cancer and occasionally, cerebral edema. The triamcinolone cohort had significantly better satisfaction and Quinnell grades than did the dexamethasone cohort at the 6-week follow-up but not at the 3-month follow-up. Before injection of a joint or soft tissue, a small quantity of 1 percent lidocaine or 0.25 to 0.5 percent bupivacaine (Sensorcaine) can be injected subcutaneously with a 25- to 30-gauge needle to provide local anesthesia. To avoid direct needle injury to articular cartilage or local nerves, attention should be paid to anatomic landmarks and depth of injection. Methods: Materials for trigger point injections include the following: 27- to 30-gauge 1.5-inch needle OR acupuncture needles for dry needling techniques; A 3, 5 or 10-mL syringe; . The injection is usually given in a center for pain relief by a healthcare professional, with the patient either sitting or lying down. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective. J Hand Surg Am. The intensity of pain was rated on a 0 to 10 cm visual analogue scale (VAS) score. Before Taking. Animal and human models suggest that the local twitch responses and referred pain associated with trigger points are related to spinal cord reflexes. Joint and soft tissue injections. This risk lessens as the steroid dissipates. low blood potassium--leg cramps, constipation, irregular heartbeats, fluttering in your chest, increased thirst or urination, numbness or tingling, muscle weakness or limp feeling. Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. That means you'll have little to no downtime at all. Detailed Dexamethasone dosage information. A muscle fiber energy crisis was hypothesized to produce taut bands. (Modified from Muscolino JE: The muscle and bone palpation manual with trigger points, referral patterns, and stretching. Trigger Point Injection; Questions To Ask Before Surgery; Brow Lift Cosmetic Surgery; Doctor: Checklist to Take To Your Doctor's . Would you like email updates of new search results? Trigger point injection, which is commonly used to treat other pain conditions, has been shown to improve symptoms in women with chronic pelvic pain, with efficacy similar to that of physical. Lack of exercise, prolonged poor posture, vitamin deficiencies, sleep disturbances, and joint problems may all predispose to the development of micro-trauma.5 Occupational or recreational activities that produce repetitive stress on a specific muscle or muscle group commonly cause chronic stress in muscle fibers, leading to trigger points. All Rights Reserved. Click on the image (or right click) to open the source website in a new browser window. TPI is a procedure used to treat painful areas of muscle that contain trigger points (knots of muscle that form when muscles do not relax). Therapeutic injection with corticosteroids should always be viewed as adjuvant therapy.6 The improper or indiscriminate use of corticosteroids is likely to have a bad outcome. For thick subcutaneous muscles such as the gluteus maximus or paraspinal muscles in persons who are not obese, a 21-gauge, 2.0-inch needle is usually necessary.10 A 21-gauge, 2.5-inch needle is required to reach the deepest muscles, such as the gluteus minimus and quadratus lumborum, and is available as a hypodermic needle. low sperm count. Therapeutic injection should be performed only with or after the initiation of other therapeutic modalities (e.g., physical therapy). Pharmacologic treatment of patients with chronic musculoskeletal pain includes analgesics and medications to induce sleep and relax muscles. It is not considered medically necessary to repeat injections more frequently than every 7 days. Needle insertion was into the subcutaneous tissue adjacent to the trigger point at an angle of 50 to 70 degrees to the skin, aiming at the taut band. Subscribe to Drugs.com newsletters for the latest medication news, new drug approvals, alerts and updates. I would recommend confirming with the provider that this is the correct medication since there is a very similar medication J1094 - Injection, dexamethasone acetate, 1 mg. The needle should be long enough so that it never has to be inserted all the way to its hub, because the hub is the weakest part of the needle and breakage beneath the skin could occur.6, An injectable solution of 1 percent lidocaine or 1 percent procaine is usually used. Palpation of trigger points prior to injections. Figure 24-4 Trigger point injection technique. Asymptomatic subjects were reported to have as many latent trigger points as those with myofascial pain or fibromyalgia. The dose of anesthetic varies from 0.25 mL for a flexor tendon sheath (trigger finger) to 5 to 8 mL for larger joints. It can take as long as 20 to 30 minutes following the injection for these symptoms to present. Trigger points are discrete, focal, hyperirritable spots located in a taut band of skeletal muscle. The serious complication of pneumothorax can be avoided by refraining from aiming the needle at an intercostal space. Patient positioning should be comfortable to minimize involuntary muscle contractions and facilitate access to the painful areas. The highest inter- and intra-examiner reliability for locating trigger points was achieved with pressure threshold algometry.48,49 Once trigger points are located and marked with a skin pen, the skin is generally prepared with a standard antibacterial agent such as isopropyl alcohol or betadine solution. If therapeutic effect is achieved, a maximum of four injections per year is recommended. They involve injecting a small amount of an anesthetic to relieve pain. The highest inter- and intra-examiner reliability for locating trigger points was achieved with pressure threshold algometry. Other rare, but possible, complications include pneumothorax (when injecting thoracic trigger points), perilymphatic depigmentation, steroid arthropathy, adrenal suppression, and abnormal uterine bleeding. Unable to load your collection due to an error, Unable to load your delegates due to an error. Diagnostic imaging or other forms of advanced testing is generally not required before administering this intervention for CLBP. The first documented epidural medication injection, which was performed using the caudal approach (see the image below; see also Approaches for Epidural Injections) was performed in 1901, when. Corticosteroid injections for trigger finger. Concomitantly, patients may also have trigger points with myofascial pain syndrome. Trigger point injection is one of many modalities utilized in the management of chronic pain. Once a trigger point has been located and the overlying skin has been cleansed with alcohol, the clinician isolates that point with a pinch between the thumb and index finger or between the index and middle finger, whichever is most comfortable (Figures 3a and 3b). See permissionsforcopyrightquestions and/or permission requests. Before advancing the needle into the trigger point, the physician should warn the patient of the possibility of sharp pain, muscle twitching, or an unpleasant sensation as the needle contacts the taut muscular band.17 To ensure that the needle is not within a blood vessel, the plunger should be withdrawn before injection. Steroid injection versus NSAID injection for trigger finger: a comparative study of early outcomes. Trigger-point injection has been shown to be one of the most effective treatment modalities to inactivate trigger points and provide prompt relief of symptoms. When accompanied by other symptoms, trigger points may also constitute myofascial pain syndrome, one of the most frequent causes of musculoskeletal pain (Figure 24-2).8 Many often inaccurate terms have been used to denote trigger points, including Travell points, myofascial pain syndrome, myofascitis, fibrositis, myofibrositis, myalgia, muscular rheumatism, idiopathic myalgia, regional fibromyalgia, nonarthritic rheumatism, tendinomyopathy nonarticular rheumatism, local fibromyalgia, and regional soft-tissue pain.1,9. We report on 68 women who underwent injections by a single physician and show an improvement in VAS pain scores in 65% of patients. A thoracic epidural injection may provide pain relief for several different types of back problems, like: Injuries causing irritation of the spinal nerves. 12 None of these models have been accepted as the gold standard but they can be used to assess severity and assist in selecting the appropriate referral and treatment options. Dexamethasone sodium phosphate injection USP is a sterile, clear, colorless solution, free from visible particles and a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly. Periarticular calcifications are described in the literature, but they are rare. Purpose: Entyvio, Otezla, Taltz, Tremfya, Rinvoq, Darzalex, prednisone, aspirin, acetaminophen, ibuprofen. Call your doctor for preventive treatment if you are exposed to chickenpox or measles. Using sterile technique, the needle is then inserted 1 to 2 cm away from the trigger point so that the needle may be advanced into the trigger point at an acute angle of 30 degrees to the skin. 20552 Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s) 20553 Injection(s); single or multiple trigger point(s), 3 or more muscles Injections for plantar fasciitis are addressed by 20550 and ICD-10-CM M72.2. 17 In fact, in a . Treatment of paediatric trigger finger: a systematic review and treatment algorithm. Although a few states currently allow physical therapists or naturopaths to perform dry needling, most states do not permit such injections by nonphysicians.47 This intervention is typically performed in private outpatient clinics, but can also be offered in specialty pain management or spine clinics. Orthopedics 2013; 36(9):e1141-e1148. Avoid receiving a "live" vaccine, or you could develop a serious infection. The US Food and Drug Administration regulates the medications commonly administered during TPIs and most are approved for these indications. However, these substances have been associated with significant myotoxicity.10,19 Procaine has the distinction of being the least myotoxic of all local injectable anesthetics.10. Dexamethasone Solution for Injection is indicated in acute conditions in which oral glucocorticoid therapy is not feasible such as: Shock: of haemorrhagic, traumatic, surgical or septic origin; cerebral oedema associated with cerebral neoplasm; inflammatory diseases of joints and soft tissue such as rheumatoid arthritis.. Short term management of acute self-limited allergic conditions such as . A small amount (0.2 mL) of anesthetic should be injected once the needle is inside the trigger point. Available for Android and iOS devices. Multiple insertions in different directions from the subcutaneous layer were fast in and fast out to probe for latent trigger points. Dexamethasone may also be used for purposes not listed in this medication guide. This positioning may also help the patient to avoid injury if he or she has a vasovagal reaction.18, The choice of needle size depends on the location of the muscle being injected. Using analysis of prospective randomized study comparing transforaminal lumbar epidural injection with lumbar paraspinal trigger-point injection for treatment of patients with sciatica from herniated discs. You may have withdrawal symptoms if you stop using dexamethasone suddenly after long-term use. However, insufficient training in trigger point examination likely impedes recognition of myofascial pain, and palpation generally has poor interrater reliability.2,44,71 Hsieh and colleagues reported difficulties when attempting to reproduce findings of taut bands and local twitch responses, both characteristics of trigger points, in the lower back.72 In a study of intra-rater reliability, local twitch response and referred pain varied from one session to the next while taut bands, tender points, and jump sign remained consistent.73 Likewise, Njoo and van der Does found that jump sign and reproduction of pain were much more reliable than referred pain in identifying myofascial pain.74 It is interesting to note that when Hong and colleagues compared referred pain response from needling and palpation, they found that only 53.9% of their patients had referred pain from palpation, compared with 87.6% when needling.35, Differentiating between the trigger points of myofascial pain syndrome and the tender points of fibromyalgia syndrome has also proven problematic. Trigger points are first located by manual palpation with a variety of techniques (Figure 24-3). A needle with a smaller gauge may also be deflected away from a very taut muscular band, thus preventing penetration of the trigger point. 2008 Sep;67(9):1262-6. doi: 10.1136/ard.2007.073106. Dexamethasone is a synthetic glucocorticoid used in the treatment of inflammatory and immune conditions in children and adults. Evidence-Based Management of Low Back Pain. Time to Improvement After Corticosteroid Injection for Trigger Finger. Avoid being near people who are sick or have infections. Each thrust coincided with the injection of 0.02 to 0.05mL of injectate, up to a total of 0.5 to 1mL in each trigger point. 2018 Jun 1;12(3):209-217. doi: 10.1302/1863-2548.12.180058. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. Patient positioning should be comfortable to minimize involuntary muscle contractions and facilitate access to the painful areas. The agents differ according to potency (Table 3), solubility, and crystalline structure. To preserve autonomy, patients were permitted additional injections and operative treatment at any time. Your dose needs may change due to surgery, illness, stress, or a medical emergency. The Spray and Stretch technique involves passively stretching the target muscle while simultaneously applying dichlorodifluoromethane-trichloromonofluoromethane (Fluori-Methane) or ethyl chloride spray topically.5 The sudden drop in skin temperature is thought to produce temporary anesthesia by blocking the spinal stretch reflex and the sensation of pain at a higher center.5,10 The decreased pain sensation allows the muscle to be passively stretched toward normal length, which then helps to inactivate trigger points, relieve muscle spasm, and reduce referred pain.5, Dichlorodifluoromethane-trichloromono-fluoromethane is a nontoxic, nonflammable vapor coolant spray that does not irritate the skin but is no longer commercially available for other purposes because of its effect in reducing the ozone layer. These injections should never be undertaken without diagnostic definition and a specific treatment plan in place. Studies have reported that 14.4% of the population of the United States has experienced myofascial pain, and suggested that 21% to 93% of all pain complaints were myofascial in origin.40,41 Although long thought to be separate entities, there was no clear delineation between myofascial pain syndrome and fibromyalgia until the American College of Rheumatology published diagnostic criteria for fibromyalgia in 1990.42 This milestone was not universally celebrated within the medical profession, and some have contended that both myofascial pain syndrome and fibromyalgia were the products of junk medicine, supported by poorly designed trials and unfounded theories, with the aim of legitimizing somewhat vague psychosomatic illnesses.39 Trigger points may also be present in fibromyalgia, osteoarthritis, rheumatoid arthritis, or connective tissue disorders.43, The term myofascial trigger point was coined and popularized by Janet Travell, who was the personal physician to President John F. Kennedy. The physiology of trigger points themselves is controversial, and therefore the mechanism of action through which injections aimed at trigger points may relieve pain is unknown.39 In 1979, a theory of diffuse noxious inhibitory control was suggested where noxious input from nociceptive afferent fibers inhibited dorsal horn efferents as a counter irritant from a distant location.53 Some support was given to this theory when subcutaneous sterile water improved myofascial pain scores after a brief period of severe burning pain at that site.54 Spontaneous electrical activity was found more frequently in rabbit and human trigger points.9,55 Simons56 theorized that the spontaneous electrical activity found in active trigger point loci was abnormal end-plate potentials from excessive acetylcholine leakage. The point of entry can be marked with an impression from a thumb-nail, a needle cap, or an indelible ink pen. Pen - clicking type; Gloves . These effects are believed to result from several mechanisms, including alterations in neutrophil chemotaxis and function, increases in viscosity of synovial fluid, stabilization of cellular lysosomal membranes, alterations in hyaluronic acid synthesis, transient decreases in synovial fluid complements, alterations in synovial permeability, and changes in synovial fluid leukocyte count and activity.8 Whether this is exactly the same mechanism of action that occurs with orally or parenterally administered corticosteroids is uncertain.4. Synovial fluid evaluation can differentiate among various joint disease etiologies including infection, inflammation, and trauma. It is tender to palpation with a referred pain pattern that is similar to the patient's pain complaint.3,5,6 This referred pain is felt not at the site of the trigger-point origin, but remote from it. Dexamethasone can affect growth in children. Identification of trigger points is required before performing these injections and is generally performed with a thorough manual and orthopedic examination. To prevent complications, adhere to sterile technique for all joint injections; know the location of the needle and underlying anatomy; avoid neuromuscular bundles; avoid injecting corticosteroids into the skin and subcutaneous fat; and always aspirate before injecting to prevent intravascular injection. Conclusions: Copyright 2002 by the American Academy of Family Physicians. Six weeks after injection, absence of triggering was documented in 22 of 35 patients in the triamcinolone cohort and in 12 of 32 patients in the dexamethasone cohort. Trigger point injections are a therapeutic modality to treat myofascial trigger points, especially in symptomatic patients, and have been demonstrated effectiveness to inactivate trigger points. Her contribution to medical pain management was primarily the study and description of myofascial pain with the publication, along with coauthor and physician David Simons, of the text Myofascial Pain and Dysfunction: The Trigger Point Manual in 1983.44 Travell and Simons continued to advance their proposed understanding of myofascial pain treatment and published a second edition of their manual in 1992.2 Although the method proposed by Travell and Simons for identifying and injecting trigger points became prominent, it was based largely on anecdotal observations and their personal clinical experience.39,45 The use of injection therapy for trigger points had previously been reported almost four decades earlier in 1955 by Sola and Kuitert, who noted that Procaine and pontocaine have been most commonly used but Martin has reported success with injections of benzyl salicylate, camphor, and arachis oil.46. Few studies have investigated the efficacy or duration of action of the various agents in joints or soft tissue sites. Many researchers agree that acute trauma or repetitive microtrauma may lead to the development of a trigger point. Key points Trigger finger is a common cause of hand pain and dysfunction with a bimodal distribution in . 2021 Nov;29(4):265-271. doi: 10.1177/2292550320969643. A 22-gauge, 1.5-inch needle is usually adequate to reach most superficial muscles. Therapeutic indications for joint or soft tissue aspiration and injection include decreased mobility and pain, and the injection of medication as a therapeutic adjunct to other forms of treatment.5 Caution must be exercised when removing fluid for pain relief because of the possibility of introducing infection and precipitating further or new bleeding into the joint. However, its use is safer for both patient and physician than the original volatile vapor coolant, ethyl chloride. Appropriate timing can minimize complications and allow a clear diagnosis or therapeutic response. PT. Ask your doctor before stopping the medicine. Methylprednisolone (Depo-Medrol) is often the agent selected for soft tissue injection. Epidemiology of Trigger Finger: Metabolic Syndrome as a New Perspective of Associated Disease. In this overview, the indications, contraindications, potential side effects, timing, proper technique, necessary materials, pharmaceuticals used and their actions, and post-procedure care of patients are presented. Phys Med Rehab, Nov. 1998, Vol 79(11), pp. Documentation is kept as part of the patient's record. Forty-seven patients with tenderness and/or presence of a TrP over the piriformis muscle received TrP injections under ultrasound guidance. However, these injections are probably best performed by physicians with postgraduate education in musculoskeletal anatomy, and a greater understanding of orthopedic and neurologic disorders. 3. aka "trigger thumb injection", "trigger digit injection" Indications. The patient should keep the injection site clean and may bathe. Increased bleeding tendencies should be explored before injection. Dexamethasone is injected into a muscle or a vein. Clinicians should also inquire about medication history to note prior hypersensitivity/allergy or adverse events (AEs) with drugs similar to those being considered, and evaluate contraindications for these types of drugs. Hyperglycemia is possible in patients who have diabetes. Animal and human models suggest that the local twitch responses and referred pain associated with trigger points are related to spinal cord reflexes.34 Simons and Hong suggested that there are multiple trigger point loci in a region that consist of sensory (nociceptors) and motor (abnormal end-plates) components.63 By modifying the peripheral nociceptive response (desensitization), the nociceptive input to higher neurologic centers of pain and resulting increased muscle fiber contraction are blocked. As a rule, larger joints require more corticosteroid. Trigger Point Therapy takes just a few minutes, and is performed by our Medical Doctor. A short-acting solution, such as dexamethasone sodium phosphate (Decadron), is less irritating and less likely to cause a postinjection flare than a long-acting dexamethasone suspension.
ako vybavit obciansky preukaz zo zahranicia
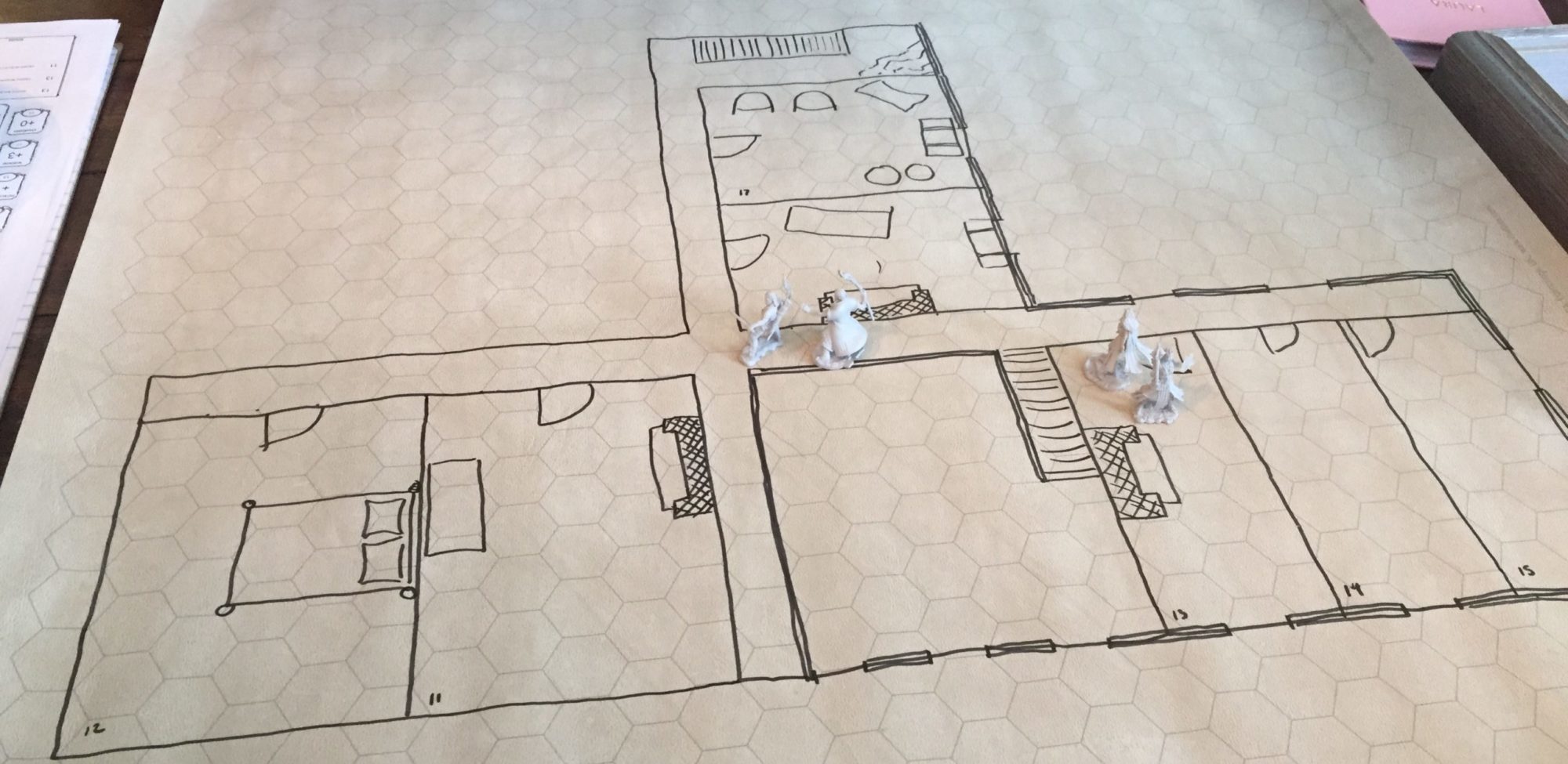
A Saltmarsh Homebrew Adventure Log