The principle by which the nurse is motivated is beneficence, not justice. This site needs JavaScript to work properly. Autonomy, as recognized by Amnesty International, is the right to make choices free from outside pressure or violence, whether mental or physical [18]. States have enacted these laws based on two theories. In the case of danger to others, social exclusion and loss of . The technicians comment disregards the seriousness of the patients illness. 2022-02-14T10:52:49-08:00 New York, NY: Oxford. Special attention is paid to boundary violations and topics including informed consent, confidentiality, mandated reporting, and HIPAA. The behaviours described in the other options are not sufficient to require involuntary hospitalization. No effect by 1315. Justification for why a patient was secluded should be recorded, along with interventions attempted in an effort to avoid seclusion. File a written report with the agencys ethics committee.d. Euthanasia is broadly defined as intentionally ending the life of a person who is suffering from a terminal or incurable illness, with the person's consent, in order to relieve their pain and suffering. This could include initiating processes that may result in involuntary admission to a psychiatric facility. For the purposes of this essay, physician-assisted suicide 1 (PAS) will be . It is essential that the rights of . Forced sterilization is a sterilization procedure, such as tubal ligation, performed without informed consent from the patient [3]. Careers. Show transcribed image text Expert Answer 1st step All steps Answer only Step 1/2 Involuntary treatment vi. The individual must be exhibiting behavior that is a danger to themselves or others and a court order must be received for more than a short (e.g. 42 0 obj Material. In this case, withholding treatment can violate the principle of justice. For example, a court could assess testimony and evidence from clinicians that a person has such a severe substance use disorder that he repeatedly loses consciousness, will not accept assistance and risks freezing to death outside. Involuntary hospitalization also protects other individuals in society. In November 2022, for example, New York City Mayor Eric Adams announced a plan to use mental health laws to facilitate involuntary treatment when people are unable to care for themselves, or when their actions endanger others. After sterilization, women sometimes become social outcasts who are banned from family activities, weddings, and funerals [29]. A nurse prepares to administer a scheduled injection of haloperidol decanoate (Haldol) to an outpatient with schizophrenia. In some situations, disclosure may be mandated to protect the patient, other persons, or public health. <><>20 21]/P 20 0 R/Pg 49 0 R/S/Link>> Interpretations of legal criteria for involuntary psychiatric admission: a qualitative analysis. Englewood Cliffs, NJ: Prentice-Hall. The nurse opens and reads a letter a patient left at the nurses station to be mailed.d. Many HIV-positive women in South Africa, Namibia, and Chile are sterilized without their knowledge or are compelled to accept the procedure to receive food or necessary medical treatment [1, 2, 4]. Please enable it to take advantage of the complete set of features! the Department of Psychiatry, University of Pittsburgh, School of Medicine, Law and Psychiatry Program, Western Psychiatric Institute and Clinic, 3811 O'Hara Street, 15213, Pittsburgh, PA, You can also search for this author in Voluntary treatment, some of them contend, is just as effective but preserves autonomy and the freedom to choose or decline treatment. Copyright 2023 American Medical Association. Beyond medical paternalism and patient autonomy: A model of physician conscience for the physician-patient relationship.Annals of Internal Medicine, 98 243248. The Negative Right to Shelter. - commits to assess quotations and offers fairly, based on non-discrimination, equal treatment, transparency, and confidentiality principles; - recalls that no payment, favor, gift, loan or any other kind of retribution is requested to submit any quotation or offer to ACTED. The https:// ensures that you are connecting to the Civil commitment aims to improve the well-being of individuals and communities. Tnnsj T. Coercive care: the ethics of choice in health and medicine. Chodoff, P. (1984). Vicarious liabilityd. The south was the most notorious in its treatment of slaves and slaves would run away. https://doi.org/10.1007/BF00819351. Respect nursepatient relationship confidentiality. An individual who does not keep an outpatient appointment with the mental health nurse.d. 39 0 obj Therefore, ethical principles should be seriously considered before drawing an ethical conclusion. Euthanasia can be voluntary, non-voluntary, or involuntary, and it can be active or passive. Rockville, MD: US DHEW. Restraint is not indicated because a patient uses profanity; there are other less restrictive ways to deal with this behaviour. After 17th court hearing, woman with TB ordered to jail for refusing treatment Washington judge issued an arrest warrant and ordered her to involuntary detention. First, under the doctrine of parens patriae, a Latin phrase that means "parent of the nation," states have a legal and ethical obligation to. The Code of Ethics for Nurses requires intervention. ANS: BIt is the health care providers duty to warn or notify an intended victim after a threat of harm has been made. Omaha, Nebraska 6th ed. ANS: DDocumentation must be specific and detail the key aspects of care. The nurse rushes after the patient and convinces the patient to return to the unit.d. Open Society Foundations. An individual diagnosed with major depression who stops taking prescribed antidepressant medication. Beauchamp, T.L., McCullough, L.B. Secondly, a number of issues relating to background factors affecting decisions for or against involuntary treatment were also discussed. Case studies through out the learning materials highlight key learning points. View the full answer Step 2/2 Final answer Transcribed image text: Second, in public health law, the concept of police power means that states have a duty to pass and enforce laws to preserve public health and safety, which can be impacted by homelessness. Describe ethical decision-making including such important considerations as risk tolerance, cultural humility, and specific decision-making models. Scand J Caring Sci. Involuntary treatment and care involves the use of coercive measures for reasons of safety or for therapeutic reasons. I am obligated to share that information with the treatment team.c. Its data found that this population commits dramatically higher rates of vandalism, arson, assault and burglary as well, although there are few nationwide studies. Opinion 8.08 Informed consent. Learn more about Institutional subscriptions. She recommends that, in addition to fines and incarceration, the medical license of health care workers be suspended or revoked if they perform sterilization without informed consent [32]. Can I download the materials, and then take the test afterwards instead of sitting in front of the computer? Select the answer with the correct rationale. Curr Opin Psychiatry. The Daily Record During the initial assessment process, the person receives care in a hospital, where clinicians determine their medical needs. Specifically, the subordinate social status of South African women hinders their ability to negotiate safer sex or participate in the workforce, factors that may make a woman feel compelled to remain in a relationship with an HIV-positive partner and that heighten vulnerability to HIV [25]. But people with severe mental illness or substance use disorder may experience impairment in their ability to deliberate, assess their needs and make decisions, which compromises their autonomy. Tobin Klusty is pursuing a JD at DePaul University College of Law in Chicago. Plan: Maintain seclusion for 8 hours and keep these two patients away from each other for 24 hours.b. In addition, medical staff should be educated on the issue and trained to provide adequate information for the patient to give informed consent [32]. Fulfill the request promptly.b. -, Matthews E. Autonomy and the psychiatric patient. Ethical acceptability of involuntary isolation and detention -2 Safeguards should be applied to the manner in which involuntary isolation or detention is implemented Applicable ethical and human rights principles must be considered and applied in the very rare cases where involuntary isolation and detention is being considered Clinical information should not be released without the patients signed consent for the release unless there is evidence of harm to self or others. 5 0 obj 2004 - 2023 Ce4less Inc All rights reserved. The distracters are incorrect and part of the stigma of mental illness. <> Permission from members of the health care team who participate in treatment planning.d. The use of seclusion or restraint to control the behavior of a client who is at risk of harming self or others gives rise to conflict between which ethical principles? Involuntary treatment was generally seen as an unwanted exception to standard care. At the discretion of the psychiatristc. A peer has difficulty writing measurable outcomes.b. Unnecessary seclusion may result in a charge of false imprisonment. uuid:918915b9-b36b-11b2-0a00-d02ab307fc7f Thanks for the idea, but its important to treat patients as individuals. Violation of the patients right to be treated with dignity and respect.c. Court-mandated treatment could include therapy, social workers, housing referrals, medication or other interventions, either in hospitals or on an outpatient basis. Vital signs stable.b. Patient safety in inpatient mental health settings: a systematic review. Read the "This principle of judicial restraint includes recognition of the inability and undesirability of the judiciary substituting its notions of correct policy for that of a popularly elected Legislature." Zayre Corp. v. Attorney Gen., 372 Mass. The University of Californias California Policy Lab analyzed surveys of 64,000 people who were homeless across 15 different states and found that 78% of the unsheltered homeless suffered from mental illness and 75% from a substance abuse disorder. imagenes biblicas para whatsapp. Her recent research focuses on deaf and hard of hearing populations, especially in the areas of behavioral health, intimate partner violence, telemental health, and help-seeking. Involuntary hospitalization of the mentally ill as a moral issue.American Journal of Psychiatry, 141 384389. 2023 Springer Nature Switzerland AG. This is clearly a pressing ethical problem that reflects global discrimination against women with HIV. As traditionally conceived, the right to shelter is a positive rightan enforceable entitlement to have the government provide or fund a temporary shelter . The site is secure. The plan of care for a patient is not completed within 24 hours of the patients admission.b. Perhaps especially where such matters are hotly debated by those . Respect my rights, respect my dignity: module three sexual and reproductive rights are human rights. Lets tell dietary to prepare popular choices and send them to our unit. Select the nurses best response. The price of failure of informed consent law: coercive sterilizations of HIV-positive women in South Africa. The World Medical Associations (WMA) International Code of Medical Ethics lists several duties that physicians are expected to uphold regardless of the geographic locations of their practices: to respect a competent patients right to accept or refuse treatment, not allow [clinical] judgment to be influenced byunfair discrimination, respect the rights and preferences of patients, act in the patients best interest when providing medical care and owe his/her patients complete loyalty and all the scientific resources available to him/her [20]. The patient who sold and distributed illegal drugsd. 2. Encourage the patient to revise the directive in light of the current health problem. Accessed August 3, 2015. 2018 Sep;32(3):1237-1246. doi: 10.1111/scs.12548. Select the best documentation. This principle states that every person has the right to make informed decisions about their healthcare and that healthcare professionals should not impose their own beliefs or decisions upon their patients. Thibaut B, Dewa LH, Ramtale SC, D'Lima D, Adam S, Ashrafian H, Darzi A, Archer S. BMJ Open. 2023 Feb;30(1):71-85. doi: 10.1177/09697330221111447. An individual who throws a heavy plate at a waiter at the direction of command hallucinations. Mann K, Grschel S, Singer S, Breitmaier J, Claus S, Fani M, Rambach S, Salize HJ, Lieb K. BMC Psychiatry. Staying with a patient demonstrating a high level of anxiety. Others contend it is cruel and coercive. Administration in Mental Health 15, 110119 (1987). She holds a Master of Social Work degree from The University of Michigan Ann Arbor, and a Doctor of Philosophy in Education and Counseling from the University of Rochester. Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Identify the dynamics of dual relationships and the ethical violations related to sexual relationships with clients. Safety is important, but less restrictive measures should be tried first. Author: Heidi Dalzell, PhD, Teresa Crowe, MSW, PhD, and Beth Russell, PhD. However, you can double check by selecting your, You can download all the required materials above where it says "Preview the material". Culver, G.M., Gert, B. Cases concerning suicidal patients and psychotic patients who did not realise their need for care were typically held as paradigmatic examples of justified involuntary care. AppendPDF Pro 6.3 Linux 64 bit Aug 30 2019 Library 15.0.4 However, as a patient advocate, the nurse is responsible for weighing factors related to the patients wishes and best interests. 4. It was moreover argued that organisational factors sometimes led to decisions about compulsory treatment that could have been avoided, given a more patient-oriented healthcare organisation. Critics also assert that involuntary commitment violates the principle of beneficence, because it can stigmatize homeless people with severe mental health and substance use disorders by implying that they do not belong in public. Spicker, J.H. Her ability to do so is diminished, and thus her right to autonomy is lost, if she is coerced into accepting a medical procedure. The nurses duty is to practise according to professional standards as well as intervene and protect the patient. endobj And if the justification for sterilization is not medical benefit but the public good, as can be the case [7], the duty of loyalty to the patient is violated. Refer the matter to the charge nurse to resolve.d. She made up a choice for me: 22 HIV-positive womens experiences of involuntary sterilization in two South African provinces. Epub 2014 Jul 1. ANS: BBreach of nursepatient confidentiality does not pose a legal dilemma for nurses in these circumstances because a team approach to delivery of psychiatric care presumes communication of patient information to other staff members to develop treatment plans and outcome criteria. IntroductionProfessional Codes of EthicsEthics vs LawEthical Principles ConfidentialitySocial Media and ConfidentialityConfidentiality and Minors (Age of Consent)Mandated ReportingHealth Insurance Portability and Accountability Act (HIPAA) Public Representations (Advertising)Duty to Protect (Tarasoff and Ewing)Achieving and Maintaining Competence -Cultural Competence and Non-Discrimination in Providing ServicesInformed ConsentMultiple or Non-sexual Dual RelationshipsCase ExampleGiving and Receiving GiftsBartering in Psychotherapy PracticeBusiness Relationships with Former Clientsce4less.com Unintentional Dual RelationshipsFriendships with Former ClientsPhysical Contact with ClientsOnline RelationshipsClient Role in Multiple RelationshipsTherapist Consequences for Boundary Violations Sexual Relationships with ClientsConsequences to the Therapist of Sexual Boundary ViolationsConsequences to the Client of Sexual Boundary ViolationsInvoluntary TreatmentEthical Decision-MakingTypes of Ethical DilemmasRisk ToleranceCultural Humility - A Framework for Understanding EthicsDecision-Making ModelsAvoiding Common Ethical Pitfalls and Dilemmas Summary. Numerous experiments which are performed on human test subjects in the United States are considered unethical, because they are performed without the knowledge or informed consent of the test subjects. official website and that any information you provide is encrypted Much of the reasoning focused on the consequences of ordering involuntary treatment, where risk of harm to the therapeutic alliance was weighed against the assumed good consequences of ensuring that patients received needed treatment. mesurer votre utilisation de nos sites et applications. It was a big risk, but a slave that made it to a . Callahan, D. (1984).Autonomy: A moral good, not a moral obsession.Hastings Center Report, 14 4042. The technician did not disclose clinical information. However, it was also argued that the law leaves room for individual judgments when making decisions about involuntary treatment. Afterward, the court may order a treatment plan that would outline requirements for the person to accept shelter and maintain weekly appointments such as attending therapy or drug treatment. endobj Report the request to the patients health care provider. A legal term that indicates that a person is receiving treatment voluntarily and has been provided with a basic understanding of the risks, benefits and alternatives of that treatment. If the patient threatens the life of another person. A signed consent by the patient for release of information stating specific information to be released.b. Accessed August 5, 2015. Which of the following patients meets criteria for involuntary hospitalization for psychiatric treatment? and enforce principles of conduct" (Witt 59). <> The respondents' judgments about involuntary treatment were typically in line with Swedish law on the subject. Regulatory boards are the final authority on courses accepted for continuing education credit. A patient in alcohol rehabilitation reveals to the nurse, I feel terrible guilt for sexually abusing my 6-year-old before I was admitted. Select the nurses most important action. The experiments include the exposure of humans to many . Notably, several proposals include civil commitment, also referred to as involuntary treatment, for people with severe mental illness or substance use disorders. 2013;38(6):71024. ANS: DBattery is an intentional tort in which one individual violates the rights of another through touching without consent. & Childress, J.F. These medications, developed in the 1990s, are available inexpensively even in countries without fully developed health care systems [23]. Autonomy is the right to make ones own decisions. Select all that apply. Sjstrand M, Eriksson S, Juth N, Helgesson G. Paternalism in the name of autonomy. WMA International Code of Medical Ethics. Provided by the Springer Nature SharedIt content-sharing initiative, Over 10 million scientific documents at your fingertips, Not logged in volume15,pages 110119 (1987)Cite this article. New York, NY: Oxford. endobj She is a licensed clinical social work in New York State and maintains a small private practice working with adolescents & adults. aC Ga{[#h1 imA^;_erP 2014 Oct 25;14:500. doi: 10.1186/s12913-014-0500-x. In this sense, HIV-positive status can be likened to having a history of mental illness or sexual assault: it constitutes a concealable stigmatized identity, the strain of which can manifest as depression, anxiety, and/or self-reported illness symptoms [31]. Some experts oppose using civil commitment laws and assert that states should rely on voluntary services. Ethics of Coercive Treatment and Misuse of Psychiatry Tilman Steinert, Prof.Dr.med. 2019 Dec 23;9(12):e030230. ANS: BThe nurses response to the worker should recognize patients rights to be treated with dignity and respect as well as promote autonomy. Recognize the role of ethical practice in the context of involuntary treatment. a. Four years later, the commission announced it would hear the casethe first it has admitted related to HIV-positive womens sexual and reproductive rights [17]which is still pending. A psychiatric nurse best applies the ethical principle of autonomy by doing which of the following? 23 0 obj Civil commitment laws also require due process, or a fair procedure for people to participate in the process, object and have assistance from legal counsel. Frequently increased volume on television, causing conflict with others.d. Review the directive with the patient to ensure it is current.b. Though involuntary treatment violates autonomy, it can also help people regain it through stabilization and recovery. Stone, A.A. (1975). Discuss informed consent in relation to ethics and boundaries. A 2004 study showed that 12.9 percent of sterilized HIV-positive women had been sterilized without consent and 29 percent had consented under coercion [15]. Physically placed in seclusion at 1420. Substandard institutional policies, however, do not absolve the individual nurse of responsibility to practise on the basis of professional standards of nursing care.
ako vybavit obciansky preukaz zo zahranicia
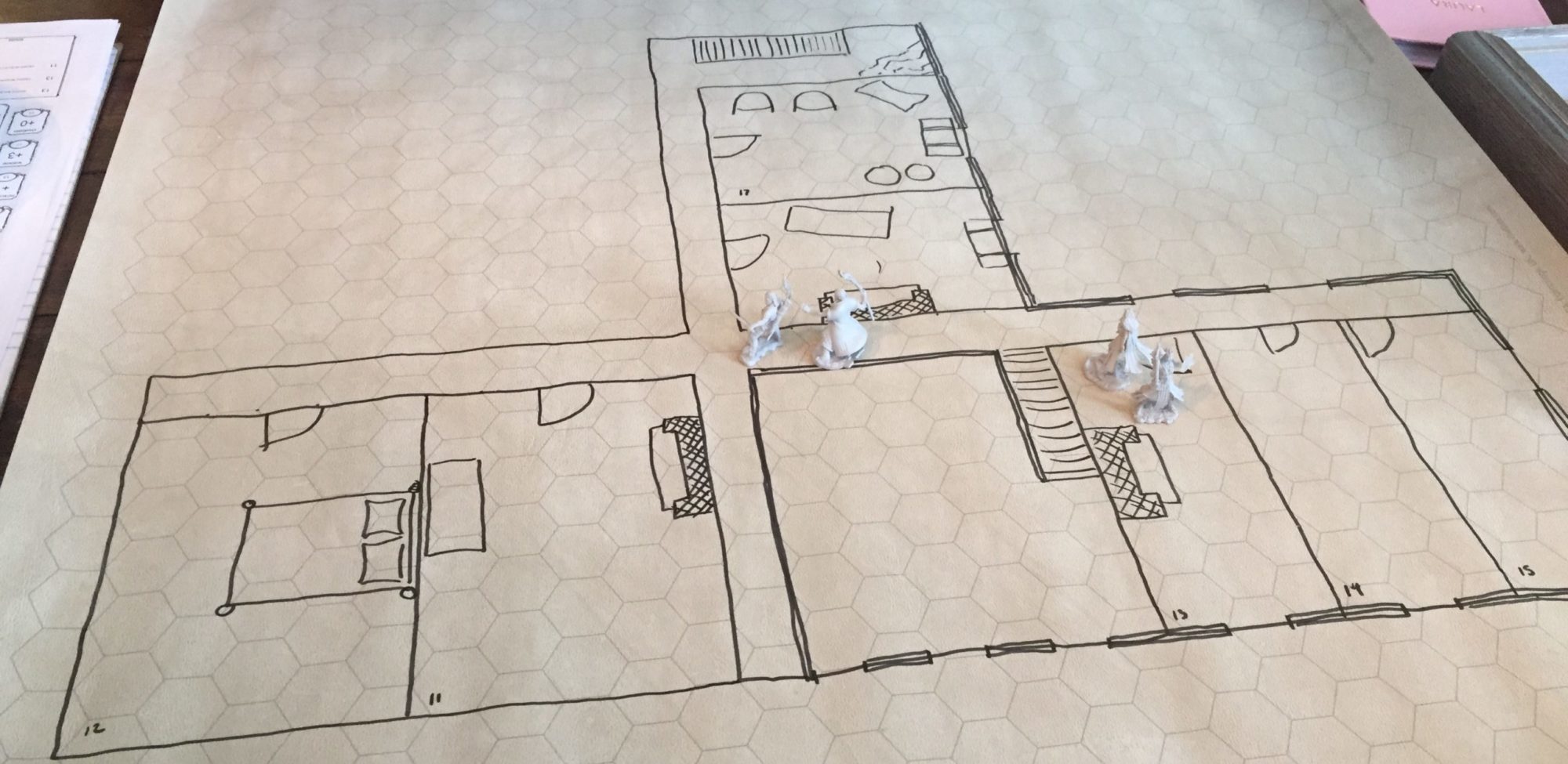
A Saltmarsh Homebrew Adventure Log